|
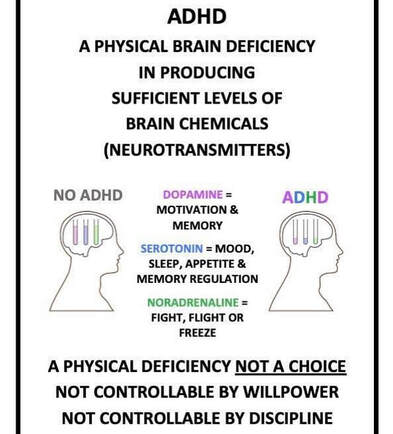
Persons who are clinically diagnosed with Attention deficit/hyperactivity disorder (ADD/ADHD) tend to regulate by doing and/or reacting. To clarify, I am referring to a reaction or behavior that is often done “impulsively” as an effort to decrease symptoms of physical discomfort and irritability (e.g overthinking, worrying, fidgeting, over-eating).
This is because there is a reduced amount of dopamine in the brain and dopamine production is neither steady or abundant in the synapses that moderate neurotransmitter production. And so, by reacting through various forms of action, the brain can enjoy a surge of dopamine, an increase in energy that improves attention, and a serotonin-based calming of restlessness. If you skipped the lecture above and want to get to the summary this is it: The ADD/ADHD brain must work harder to produce the neurotransmitters non-ADD/ADHD brains produce organically. With Eye Movement Desensitization Reprocessing (EMDR) therapy becoming popularized as a mental health treatment, I would like to spend some time with you today talking about the various mechanisms of trauma and how it affects our brain and its functioning.
A primary question I often receive centers on the question of "what is dissociation" and "will I dissociate during EMDR?". Dissociation is a survival oriented process. Dissociation is the way the brain has the ability to take something that is so overwhelming when a patient cannot escape a stressful event and/or is caught in the freeze response. So for example, there might be a child being hurt by a caregiver. Children are often too small to run away or fight back. They are the victim of the grown up. What the brain does during this type of scenario is that it allows the child to be there and not be there at the same time. In other words, the dissociative process of the brain is protecting the child so they can survive the experience. EMDR therapy helps patients move through the dissociative process, which is inherent in any kind of trauma. EMDR helps the patient move through the experience with a much reduced rate of emotional arousal. For the previous thirty years when trauma and Post Traumatic Stress Disorder (PTSD) were added to the Diagnostic Statistical Manual (DSM), it only categorized trauma as specifically large or “Big T” events. However, adverse life experiences or “little traumas” can also have a major impact on social, emotional, psychological, and physiological functioning. I personally choose not to define trauma by “little” or “big” events. What is significant to me in my professional opinion is how the smaller, more repetitive patterns of events become recorded in the nervous system and because of its repetition, these experiences gradually accumulate in the brain. Where in the brain does this all get stored? Please allow me to introduce to you, if you have not already learned about the amygdala. The amygdala is within the right hemisphere of the brain, known for responding to a heightened sense of arousal. The amygdala translates information that it receives from the other parts of the brain into an emotional response. This type of response can manifest in a variety of ways within the body (e.g. heightened blood pressure, more rapid breathing, blood moving from the central part of the body to the peripheral, and the release of adrenaline). In my next post, I will continue to discuss two key symptom behaviors that are congruent with trauma: avoidance and rumination. Stay tuned! I am a huge advocate for using a strengths-based perspective. So when I meet with someone for session, I am going to ask "what's strong in you?" rather than "what's wrong in you?"
When I would have resident physicians shadow me as a therapist in Tallahassee, I would often get asked questions that focused on finding connection with adolescents and finding ways to get to the roots of presenting mental health issues. I will never forget a specific conversation I had with a resident one day. He told me that during his rotation in the emergency room, he said he had seen an adolescent patient who attempted suicide by slitting his/her wrists and didn't know where to begin or how to begin talking to the teenager. I encouraged him to start where the patient is. Through his lens, it would have been expected of the resident to look at the physical cuts to the wrists and begin treatment there. But I invited him to acknowledge that patient, that person's pain. Yes, physical pain is obvious, but clearly that person was in a kind of pain that modern medicine, no matter how advanced, could not directly touch. That kind of pain can be more significant than any physical pain you or I can experience considering we can find refuge in knowing a blood test, IV infusion, or over the counter prescription can locate the root of the issue and give us relief. Healing begins the moment we feel heard. So why are we not making greater efforts to listen? So excited to announce that after two years of intensive training, I have been approved for certification as a Certified EMDR therapist!
What is the difference between EMDR trained and Certified? Clients will ask me, "what does it mean if I read that a therapist says he or she is Level 1 or Level 2 trained?". Generally speaking, EMDR basic trainings require a minimum of six days and a majority of EMDR trainings will break up the six day requirement by hosting two-three day weekend training events held on different assigned weekends of a specific month. When a clinician will state that he or she is "LEVEL 1 EMDR Trained", he or she has technically only completed the first three days of basic training. Subsequently, when a clinician states he or she is "LEVEL 2 EMDR Trained", he or she has completed the six days of basic training. Some therapists may find the basic training to be sufficient for what he or she is looking to add to his or her own practice. Once I completed basic training I immediately began applying the skills I learned and provided EMDR therapy in my sessions. I began to notice that my clients symptoms began to resolve almost immediately. How cool is that? People feeling better? I was hooked! After completing basic training I was presented the opportunity to invest in furthering my knowledge of EMDR treatment even more and I went for it! I dedicated the next two years of my life utilizing EMDR and somatic processing in my sessions, attending monthly meetings with an EMDRIA approved consultant for case consultation, and learning even more about the history, mechanism of action, and function of EMDR. In my down time I spent hours studying the limbic system, neurobiology of trauma, and human anatomy so that I could truly understand the biology of stress on a cellular level. My training and certification was unique in that the founder of the Somatic Attachment Focused EMDR protocol (S.A.F.E) interweaved a concept of noticing and understanding how the body will tell us what the client needs and how a feeling, movement, or overall posture may be linked to the emotion(s) associated with a disturbing memory. Being an EMDR provider requires a great depth of understanding and dedication to understanding how the human body reacts to stress, perceived danger, and how to work with a client when he or she may be beyond a window of tolerance to keep him or her safe. As a Certified EMDR therapist, part of my intensive training focused primarily on safety. This type of treatment necessitates a high level of competency and should not be used as a treatment unless the clinician has the qualifications, experience, and training to do so. I understand the necessity of keeping my clients safe and closely monitor each session, ensuring a person does not leave the session until he or she feels grounded enough to do so. So what's next? I look forward to continuing to utilize EMDR in my practice and would like to become an EMDRIA approved consultant. As a consultant, I would have the privilege of working with mental health professionals in the field who are interested in deepening his or her understanding of EMDR treatment. Regardless, the journey is far from over! If you have any questions regarding EMDR, Certification in EMDR, or would like to make an appointment, please feel free to give me a call: 904-280-8006 Do not let fear steer the wheel of your life decisions. You can accomplish a lot more looking at things through the lens of love rather than the lens of fear. Once we can acknowledge we are saying no with love instead of saying yes with fear, setting boundaries could become a lot less painful for some. Have a great start to your week!
Generally speaking, Cognitive Behavioral Therapy (CBT) works by breaking down the thoughts, images, beliefs and attitudes and how these processes relate to how a person behaves (and emotionally responds).
. . Let’s look at this model from a different lens, or a somatic lens: you experience an event your BODY responds with a feeling (e.g danger, fear, excitement, happiness, pain) feeling gets translated into thought/opinion/memory (e.g Is it safe? Is it going to be painful? Can I get hurt from it? Maybe I should post that selfie to show my ex how I’m thriving) you respond and go from there (aka your behavior) . . . What’s my point? I hear A LOT of horror stories of folks having their feelings invalidated. Your feelings are so important. YOU are important. And when you are able to identify what you FEEL you can identify the thought and if you can do that, you can do ANYTHING. Today we will go a little deeper in trauma. Dr. Stephen Porges developed Polyvagal theory to expand our understanding of how the nervous system responds to threat and trauma.
In our last post we briefly talked about the nervous system and it's role in trauma. Dr. Porges added a third factor: the vagus nerve. The vagal nerve plays a role in regulating the heart, face, stomach, and breath. The nerve also communicates with the brain. When talking about the nervous system, we will need to use some anatomical terms to orient ourselves: Ventral: towards the front of the torso. The navel (belly button) is on the ventral or anterior part of the body. Dorsal: towards the back of the torso. For example, the shoulder blades are dorsal or posterior to the ribs. The vagus nerve, or more specifically the ventral branch of the vagus nerve, controls the muscles of the face. The face, heart, and lungs are all used when we interact with others (e.g. smiling or making eye contact, feeling our heart beating faster, using our lungs to speak and breathe). This is what Dr. Porges calls "social engagement". In other words, it is through our face, heart, and brain connection that we learn to respond to interpersonal threats and challenges. Let's use a worst-case scenario as an example of how this works. Imagine this: you are walking down a dark alley alone and you see a dark shadow in the distance approaching you. Your face (eyes, nose, and ears) capture the image, hear the footsteps, and smell any scents or aromas in the air. Your brain takes in all the information your sensory organs are sending and tries to make sense of the shadowy figure. As this takes place, your heart begins pumping a lot harder to disperse blood flow to your muscles just in case you need to fight or make a run for it (flee/flight) from this unfamiliar and potentially dangerous shadowy figure. So what just happened? Your vagal nerve was working in overdrive, working hard as gatekeeper of your body's responses to the environment, moderating a conversation between your brain and body during a moment of possible danger. Another branch of the vagus, the dorsal vagus, regulates organs below the diaphragm (e.g. stomach, intestines). The dorsal vagus activates what we call "shutting down" during overwhelming trauma. Polyvagal theory emphasizes that our nervous system has more than one defense strategy and whether we use fight-or-fight or shut down, is not a decision we actively decide to use. But if we are trapped, or feel unsafe, our nervous system reads those cues and makes a decision from there. I should note these responses were adaptive to the environment or situation that an event or trauma occurred at a moment in time. This is where Somatic and Attachment-focused EMDR (Eye Movement Desensitization Reprocessing) can really help clients identify these patterns and work WITH the vagal responses to process painful memories and heal. Somatic and Attachment-Focused EMDR or SAFE EMDR model is compatible in treating most psychiatric diagnoses including but not limited to PTSD, trauma, anxiety, and depression. This concludes our discussion about the neurobiology of trauma. If you or a loved one have any questions, would like further information on EMDR, or would like to set up an appointment. Please feel free to give me a call at 904.404.1763. |
AuthorAmy Pope-Latham, LCSW is a board certified mental health professional in Ponte Vedra Beach, FL. Archives
December 2022
Categories
All
|


 RSS Feed
RSS Feed