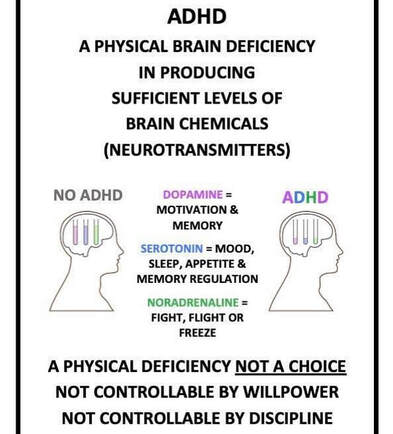
 The human body is an amazing and complex system, and understanding how it works is essential for true healing. Most people are beginning to understand the importance of physical and emotional health, but few understand the connection between the two. That connection is fascia, the connective tissue that runs throughout the body and hold every blood vessel, bone, nerve fiber, and muscle in place. Fascia is also responsible for the transmission of neurotransmitters (e.g. serotonin, dopamine, acetylcholine) throughout your body. This connective tissue transmits hormones such as adrenaline and oxytocin throughout your body as well. What does this all mean? The long and the short is that your fascia is deeply intertwined with the nervous system. Fascia plays a major role in how we physically experience stress, including traumatic events. When the body experiences trauma, it creates tension in the fascia that can cause pain and limit movement. This tension can become chronic and prevent the body from healing completely. When emotional trauma occurs, the body also responds by creating tension in the fascia. Lack of moment, emotional stress, physical injury, and previous unresolved trauma can lead to physical and physiological changes to the fascia, which is often then associated with the symptoms most frequently seen in patients with fibromyalgia, chronic fatigue syndrome, chronic pain, and inflammation. If you scroll throughout this blog, it is apparent I frequently refer to the vagus nerve in my posts. To briefly review what the vagus nerve is, the vagus nerve plays a key role in communicating changes that occur within the fascia to your brain. The vagus nerve assists in maintaining the channels of communication between the brain and body that helps regulate your autonomic nervous system (ANS). The sympathetic nervous system (SNS) which is associated with fight or flight will increase the speed at which your body wants to respond or react to stimuli and the vagus nerve provides a steady brake to slow things down. In situations that are traumatic or life threatening, this “emergency brake” can kick in abruptly, bringing you to a sudden and hard stop. Sometimes this may result in physical symptoms including nausea, dizziness, or fainting. Fascia is the largest sensory organ in your body and its primary role is to communicate information about what is happening in your body to your brain. When we experience trauma, we either move into freeze (immobility) or faint. If this trauma response does not resolve we can feel stuck and over time, lose our connection to our bodily sensations. We may feel more disconnected or dissociated. When working to heal trauma, it is so important to understand how these vital physiological and anatomical structures play a pivotal role in not only recovering from traumatic events, but to also understand how we can work with these structures using mind-body sensory awareness. The key is to progress slowly on the path towards reconnecting with your body and restoring a relationship to your body after trauma. Persons who are clinically diagnosed with Attention deficit/hyperactivity disorder (ADD/ADHD) tend to regulate by doing and/or reacting. To clarify, I am referring to a reaction or behavior that is often done “impulsively” as an effort to decrease symptoms of physical discomfort and irritability (e.g overthinking, worrying, fidgeting, over-eating).
This is because there is a reduced amount of dopamine in the brain and dopamine production is neither steady or abundant in the synapses that moderate neurotransmitter production. And so, by reacting through various forms of action, the brain can enjoy a surge of dopamine, an increase in energy that improves attention, and a serotonin-based calming of restlessness. If you skipped the lecture above and want to get to the summary this is it: The ADD/ADHD brain must work harder to produce the neurotransmitters non-ADD/ADHD brains produce organically. With Eye Movement Desensitization Reprocessing (EMDR) therapy becoming popularized as a mental health treatment, I would like to spend some time with you today talking about the various mechanisms of trauma and how it affects our brain and its functioning.
A primary question I often receive centers on the question of "what is dissociation" and "will I dissociate during EMDR?". Dissociation is a survival oriented process. Dissociation is the way the brain has the ability to take something that is so overwhelming when a patient cannot escape a stressful event and/or is caught in the freeze response. So for example, there might be a child being hurt by a caregiver. Children are often too small to run away or fight back. They are the victim of the grown up. What the brain does during this type of scenario is that it allows the child to be there and not be there at the same time. In other words, the dissociative process of the brain is protecting the child so they can survive the experience. EMDR therapy helps patients move through the dissociative process, which is inherent in any kind of trauma. EMDR helps the patient move through the experience with a much reduced rate of emotional arousal. For the previous thirty years when trauma and Post Traumatic Stress Disorder (PTSD) were added to the Diagnostic Statistical Manual (DSM), it only categorized trauma as specifically large or “Big T” events. However, adverse life experiences or “little traumas” can also have a major impact on social, emotional, psychological, and physiological functioning. I personally choose not to define trauma by “little” or “big” events. What is significant to me in my professional opinion is how the smaller, more repetitive patterns of events become recorded in the nervous system and because of its repetition, these experiences gradually accumulate in the brain. Where in the brain does this all get stored? Please allow me to introduce to you, if you have not already learned about the amygdala. The amygdala is within the right hemisphere of the brain, known for responding to a heightened sense of arousal. The amygdala translates information that it receives from the other parts of the brain into an emotional response. This type of response can manifest in a variety of ways within the body (e.g. heightened blood pressure, more rapid breathing, blood moving from the central part of the body to the peripheral, and the release of adrenaline). In my next post, I will continue to discuss two key symptom behaviors that are congruent with trauma: avoidance and rumination. Stay tuned!  I am so excited to share the news of this freshly released podcast episode with you! I recently sat down for a conversation with Jacksonville local, Kacie Main, who is both the author of her book "I Gave Up Men for Lent" and host of "The Better You" podcast. Kacie beams with joy and she is clearly passionate about learning and inspiring others. During our conversation, Kacie (with permission of course) picked my brain about my most favorite topics in mental health, including EMDR therapy, the neurobiology of trauma, and mindfulness! Click here for the link to Episode 7 of my conversation with Kacie for Apple Click here for the link for Episode 7 of my conversation with Kacie for Stitcher  This community continues to surprise me in the most incredible ways and I am so thrilled to be here in Ponte Vedra Beach knowing people like Kacie are here shaping the world into a better place. I know I for sure look forward to hearing more from Kacie. Something leads me to believe she is on to something special with the work she is doing. If you have not done so yet, please give a follow to the incredible Kacie Main Instagram account @kaciemain_writes and of course, tune into and give a follow to the podcast @thebetteryoupodcast. Your brain is not wired to make you happy. |
AuthorAmy Pope-Latham, LCSW is a board certified mental health professional in Ponte Vedra Beach, FL. Archives
December 2022
Categories
All
|


 RSS Feed
RSS Feed